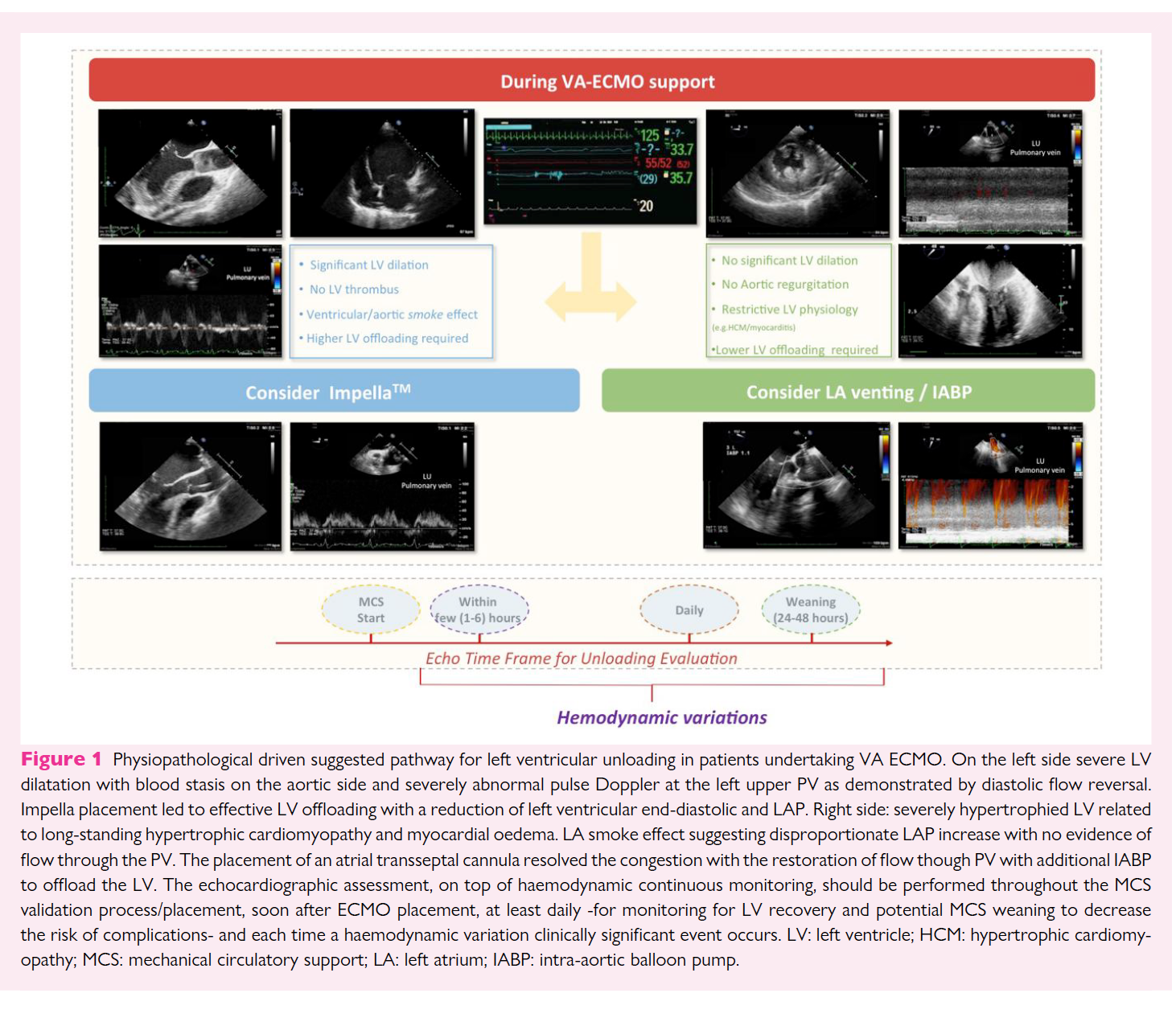
The use of peripheral veno-arterial extracorporeal membrane oxygenation (VA ECMO) in patients with refractory cardiogenic shock (CS) has become increasingly common. Although bypassing and potentially supporting almost completely cardiac and respiratory function, this ECMO configuration leads to a rise in left ventricle (LV) afterload as a consequence of the increased retrograde pressure from the femoral/iliac artery to the ascending aorta. This may result in further worsening of ventricular function, from altering ventriculo/arterial coupling and from increasing left ventricular end-diastolic pressure (LVEDP) and left atrial pressure (LAP).
Recent studies have demonstrated that early LV unloading with additional percutaneous left ventricular assist devices (pLVAD) relieves ventricular distension and improves outcomes. However, the optimal unloading strategy (e.g. impella, intra-aortic balloon pump-IABP, transseptal cannulation) has not yet been defined.3,4Additionally, the criteria for the indications, timing, and mode of LV unloading (pLVAD selection), are mostly based on pathophysiology and clinical experience, rather than on high-quality evidence-based from published data. No validated indices exist or cut-off values (e.g. chamber size quantification) as patients needed VA ECMO may have a wide range of underlying cardiac morpho-functional features (e.g. CS related to acute myocardial infarction in previously normal LV or related to acute decompensated heart failure with dilated cardiomyopathy).
We aim to describe a systematic ultrasound-guided approach, integrating imaging and pathophysiological information, to select the most appropriate unloading strategy in patients with CS undergoing peripheral VA ECMO. Only percutaneous approaches will be discussed.