Setting positive end-expiratory pressure: using the pressure-volume curve
18
Dec 23
Multiorgan evaluation of perfusion and congestion using ultrasound in patients with shock
30
Sep 23
Abstract
How to unload the left ventricle during veno-arterial extracorporeal membrane oxygenation
20
Sep 23
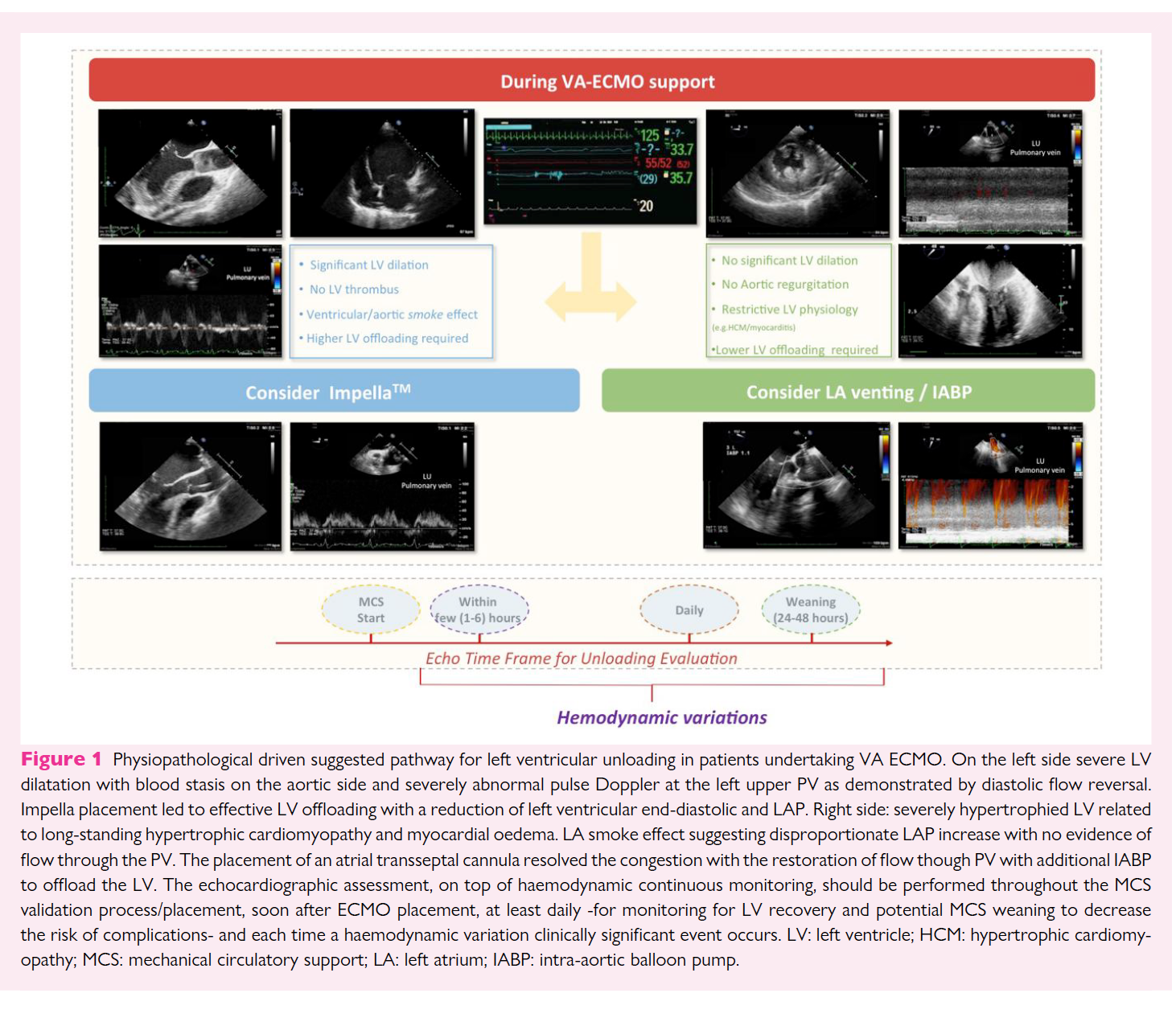
The use of peripheral veno-arterial extracorporeal membrane oxygenation (VA ECMO) in patients with refractory cardiogenic shock (CS) has become increasingly common. Although bypassing and potentially supporting almost completely cardiac and respiratory function, this ECMO configuration leads to a rise in left ventricle (LV) afterload as a consequence of the increased retrograde pressure from the femoral/iliac artery to the ascending aorta. This may result in further worsening of ventricular function, from altering ventriculo/arterial coupling and from increasing left ventricular end-diastolic pressure (LVEDP) and left atrial pressure (LAP).
Recent studies have demonstrated that early LV unloading with additional percutaneous left ventricular assist devices (pLVAD) relieves ventricular distension and improves outcomes. However, the optimal unloading strategy (e.g. impella, intra-aortic balloon pump-IABP, transseptal cannulation) has not yet been defined.3,4Additionally, the criteria for the indications, timing, and mode of LV unloading (pLVAD selection), are mostly based on pathophysiology and clinical experience, rather than on high-quality evidence-based from published data. No validated indices exist or cut-off values (e.g. chamber size quantification) as patients needed VA ECMO may have a wide range of underlying cardiac morpho-functional features (e.g. CS related to acute myocardial infarction in previously normal LV or related to acute decompensated heart failure with dilated cardiomyopathy).
We aim to describe a systematic ultrasound-guided approach, integrating imaging and pathophysiological information, to select the most appropriate unloading strategy in patients with CS undergoing peripheral VA ECMO. Only percutaneous approaches will be discussed.
Airway ultrasound to detect subglottic secretion above endotracheal tube cuff
10
Sep 23
Dynamic NLR and PLR in Predicting COVID-19 Severity: A Retrospective Cohort Study
30
Aug 23
Abstract
Introduction
The hyperinflammation phase of severe SARS-CoV-2 is characterised by complete blood count alterations. In this context, the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be used as prognostic factors. We studied NLR and PLR trends at different timepoints and computed optimal cutoffs to predict four outcomes: use of continuous positive airways pressure (CPAP), intensive care unit (ICU) admission, invasive ventilation and death.Methods
We retrospectively included all adult patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia admitted from 23 January 2020 to 18 May 2021. Analyses included non-parametric tests to study the ability of NLR and PLR to distinguish the patients’ outcomes at each timepoint. Receiver operating characteristic (ROC) curves were built for NLR and PLR at each timepoint (minus discharge) to identify cutoffs to distinguish severe and non-severe disease. Their statistical significance was assessed with the chi-square test. Collection of data under the SMACORE database was approved with protocol number 20200046877.Results
We included 2169 patients. NLR and PLR were higher in severe coronavirus disease 2019 (COVID-19). Both ratios were able to distinguish the outcomes at each timepoint. For NLR, the areas under the receiver operating characteristic curve (AUROC) ranged between 0.59 and 0.81, and for PLR between 0.53 and 0.67. From each ROC curve we computed an optimal cutoff value.Conclusion
NLR and PLR cutoffs are able to distinguish severity grades and mortality at different timepoints during the course of disease, and, as such, they allow a tailored approach. Future prospects include validating our cutoffs in a prospective cohort and comparing their performance against other COVID-19 scores.Multimodality imaging in cardiogenic shock: state-of-the art
20
Aug 23
Abstract
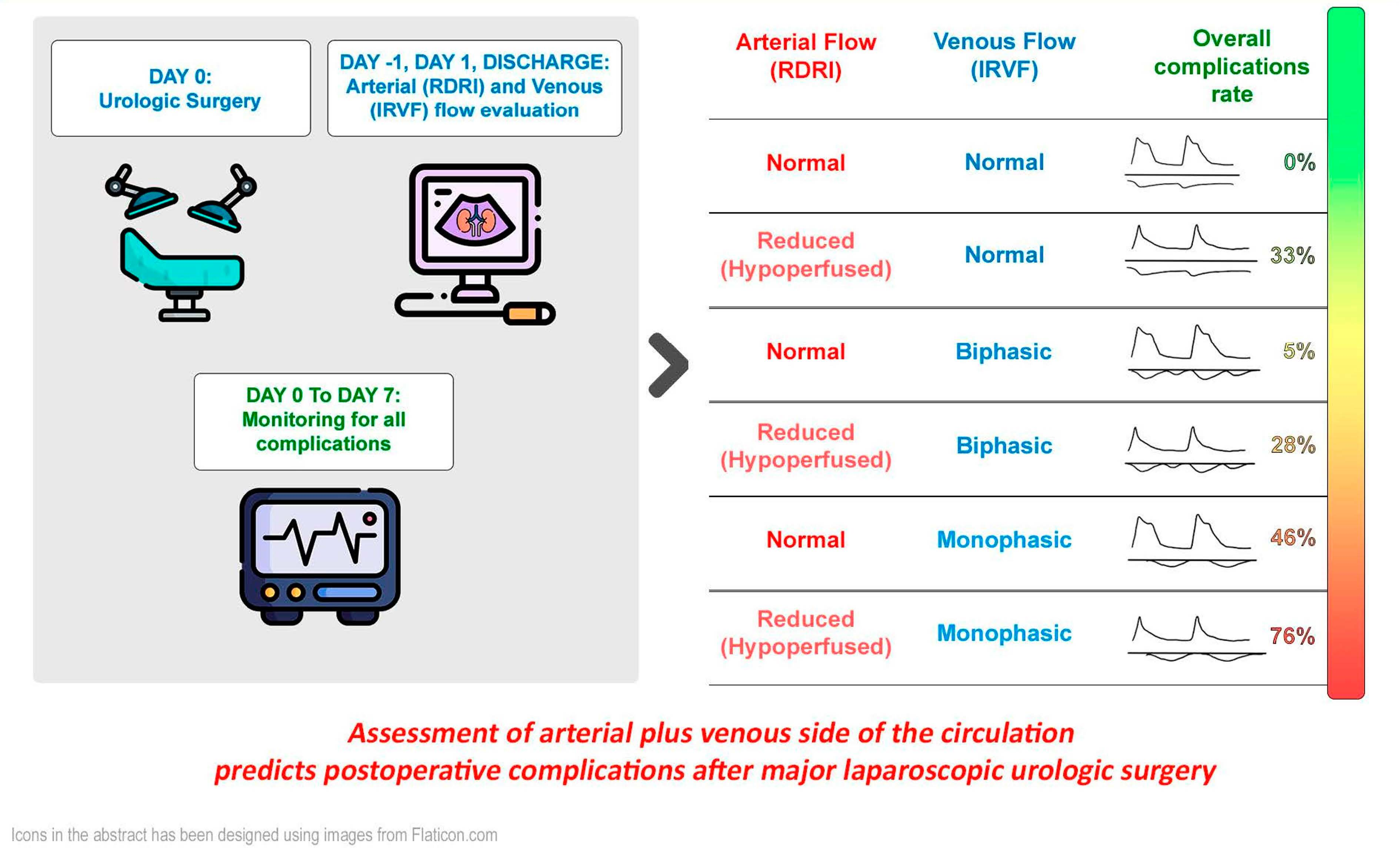
Perioperative Renal Ultrasonography of Arterio-to-Venous Coupling Predicts Postoperative Complications after Major Laparoscopic Urologic Surgery
10
Aug 23
Abstract
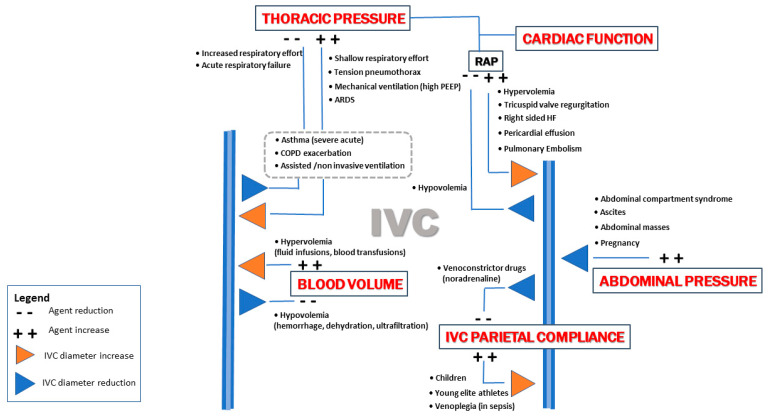
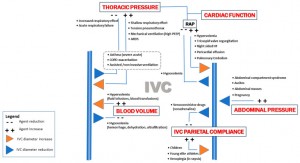
Inferior Vena Cava Ultrasonography for Volume Status Evaluation: An Intriguing Promise Never Fulfilled
6
Aug 23
Abstract
The mental health toll of COVID-19: significant increase in admissions to ICU for voluntary self-inflicted injuries after the beginning of the pandemic
31
Jul 23
Abstract
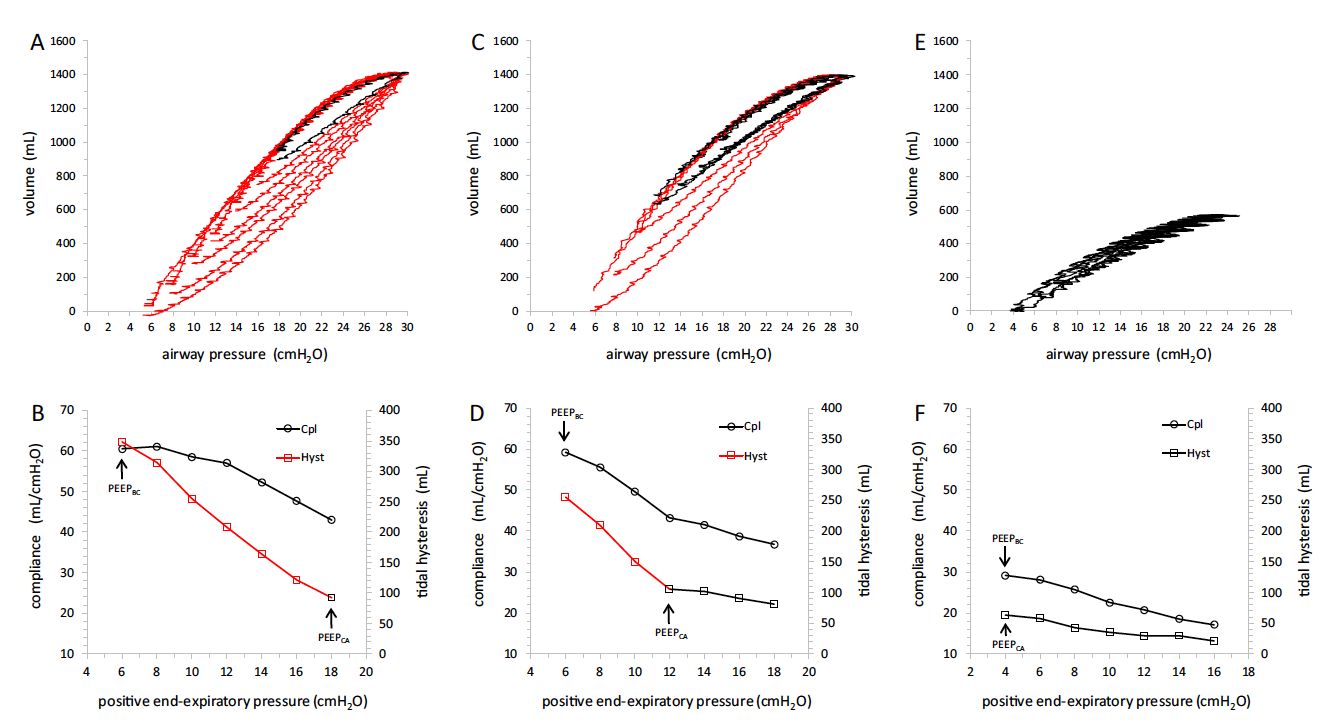
Tidal lung hysteresis to interpret PEEP-induced changes in compliance in ARDS patients
15
Jun 23